Olga Zvereva: ‘Glaucoma has no symptoms. You can’t detect it on your own!’
Ophthalmologist of the Republican Clinical Ophthalmological Hospital on the dangers of glaucoma, ways to fight it, and the role of meditation

Around 37,000 residents of Tatarstan are currently living with glaucoma — a deceptive eye disease that presents no initial symptoms and is often diagnosed at a late stage when damage is irreversible. In severe cases, it can lead to total blindness. Why does glaucoma develop? How can it be detected in time? What can doctors do if the disease is caught early? Olga Zvereva, an ophthalmologist at the Republican Clinical Ophthalmological Hospital of the Ministry of Healthcare of the Republic of Tatarstan named after Professor E.V. Adamyuk and Assistant Professor at the Department of Ophthalmology at the Kazan State Medical Academy, shared insights with our publication.
“Blindness strikes suddenly: patients may have glaucoma for 10–20 years without knowing it”
What are the statistics on glaucoma in Tatarstan? How many patients are currently diagnosed with this disease, and what is the trend in its prevalence?
The prevalence of glaucoma has not significantly increased — this is true worldwide, in Russia, and in Tatarstan. In Russia, approximately 1.25 million patients are under medical supervision for glaucoma. In Tatarstan, around 37,000 people have been diagnosed, including 11,000 in Kazan. If we compare Tatarstan’s figures with the rest of Russia, our region consistently falls in the middle range — neither above nor below average. These numbers remain stable.
However, this stability is not necessarily a positive factor, and here’s why. Experts believe that, in reality, the number of glaucoma cases worldwide is at least twice as high. This is because the disease is “silent”— it has no noticeable symptoms in its early stages. Without regular preventive eye exams, blindness can occur suddenly. Sadly, by the time a person realises something is wrong, they may have unknowingly had glaucoma for 10–20 years and only discover it in old age.

“Unfortunately, nerve damage cannot be reversed”
What are the key risk factors for blindness caused by glaucoma?
The primary risk factor is late-stage diagnosis, particularly at the third stage or beyond. As I’ve mentioned, glaucoma-related blindness typically develops over 20 years, progressing through four stages, each lasting about five years. Some patients experience faster progression, while for others, it takes longer.
This is why it’s so unfortunate when a patient only seeks medical attention after noticing significant vision loss. Glaucoma is an asymmetrical disease, usually affecting one eye first before gradually impacting the other.
Other major risk factors include a significant increase in intraocular pressure that cannot be controlled for various reasons.
Another critical issue is the delayed recommendation for surgical treatment, which remains one of the most effective ways to lower intraocular pressure. Unfortunately, many patients perceive surgery as something frightening, opting instead for prolonged medication use. As a result, surgery may be performed too late — when the optic nerve and eyeball have already sustained severe damage. Sadly, this can ultimately lead to blindness.
How does glaucoma develop, and what exactly is this disease?
Glaucoma is actually a collection of many different diseases. Our professor, Arkady Pavlovich Nesterov, described more than 80 distinct forms of this condition, all grouped under the common term “glaucoma”.
In general, glaucoma is a progressive atrophy of the optic nerve, not due to issues in the brain but rather pathological changes within the eye itself. When the outflow of intraocular fluid is disrupted, intraocular pressure rises, leading to biomechanical changes in the eye’s structures. Vascular dysfunctions develop within the eye, and, unfortunately, degenerative changes occur in the retinal ganglion cells. All these factors contribute to the progressive damage of optic nerve fibers, ultimately resulting in blindness over time.

With proper treatment, the condition of nerve fibers can improve. However, once these fibers are destroyed, there is a point of no return — beyond which no medical intervention can restore vision
Is it irreversible?
Unfortunately, nerve cells do not regenerate, and so far, all attempts to restore them — whether through stem cells or new neurotrophic factors — have not yielded meaningful results in regenerating the optic nerve.
However, when patients seek medical attention at an early stage, treatment can have a positive impact. Damaged nerve fibers that were compressed and under strain can show signs of improvement with proper therapy. But if these fibers have already died, we reach a point of no return — beyond which nothing can be done to restore vision.
“One shouldn’t wait for symptoms”
How is glaucoma diagnosed, and what are its clinical signs from a medical perspective?
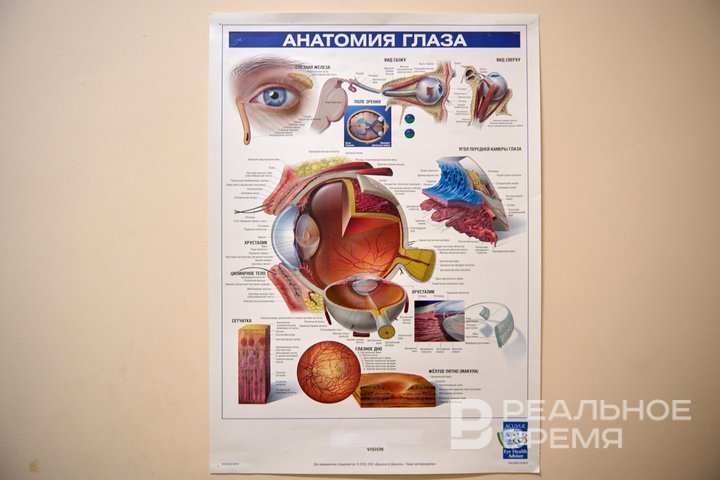
During an eye examination, an ophthalmologist always checks visual acuity, measures intraocular pressure, and examines the fundus of the eye. The fundus is the back part of the eye, where we can see the retina and the optic nerve. The condition of the optic nerve is what allows us to detect glaucoma. The doctor may notice asymmetry — differences in the optic nerve between the two eyes — and specific signs of the disease.
Interestingly, intraocular pressure is not always the primary indicator of glaucoma. A patient with high intraocular pressure may not necessarily have glaucoma (for example, they might have ocular hypertension without glaucomatous damage). Conversely, early stages of glaucoma can sometimes develop even when intraocular pressure is within normal limits. In Russia, this so-called “normal-tension glaucoma” accounts for approximately 35–40% of cases.
The key diagnostic method — fundus examination, ophthalmoscopy. If a clinic does not have an optical coherence tomograph (OCT) or a computerized perimeter, an ophthalmologist who suspects glaucoma will refer the patient to a specialized facility where these tests are available.
According to clinical guidelines, glaucoma patients must undergo computerised perimetry at least once a year.
Is it possible to suspect glaucoma by yourself?
Trying to look for symptoms on your own is usually pointless. Many patients come to us complaining of discomfort, a foreign body sensation in the eye, burning, headaches, eye strain, or fatigue — naturally assuming they have glaucoma. However, these are typically symptoms of dry eye syndrome, which affects almost all women over 50–55 years old, as well as people who spend their entire workday in front of a computer.
The real problem is that those who have no symptoms at all sometimes visit us with an advanced stage of glaucoma, already experiencing vision loss, when it becomes extremely difficult to help them.
That's why you should not wait for symptoms. Once you turn 40, you must see an ophthalmologist — whether or not you have a family history of glaucoma or relatives who lost their sight for unclear reasons. If you don’t have any serious underlying conditions (such as cardiovascular diseases, diabetes, hypertension, migraines, insomnia, or neuroses), you should still have an annual eye check-up. I repeat: even if you have no complaints! Glaucoma may already be progressing without you noticing.

You should not wait for symptoms. Once you turn 40, you must see an ophthalmologist
There are no noticeable symptoms of glaucoma! It is impossible to determine this disease independently
“By reducing intraocular pressure by 30%, we slow down the progression of glaucoma by 70%"
What are the current treatment methods for slowing down glaucoma progression?
The primary treatment focuses on lowering intraocular pressure. This is a scientifically proven approach: reducing eye pressure by 30% slows down glaucoma progression by 70%. Initially, patients are prescribed eye drops, and after a month, they return for a follow-up to assess the effectiveness and safety of the treatment. If everything is well, the patient continues regular monitoring. During the first two years, check-ups occur every three months to track the progression of the disease, the patient’s response to medication, and their treatment adherence.
If a patient comes in with an advanced (third-stage) glaucoma, surgery will likely be scheduled within six months to a year. However, before the procedure, medication is still prescribed to lower eye pressure and reduce risks. Glaucoma surgery is a minor procedure performed under local anesthesia. The goal is to create new drainage pathways to help fluid exit the eye, ultimately lowering intraocular pressure. Multiple surgeries may be required as the disease progresses.
Again, glaucoma is not merely about increased intraocular pressure. It is a neurodegenerative disease accompanied by vascular dysfunction in the eye. That’s why your ophthalmologist will likely refer you to other specialists, such as a cardiologist, neurologist, endocrinologist, or vascular surgeon. You will need to control your blood sugar levels, cholesterol, and blood pressure. These factors play a crucial role in eye health. The eye is one of the most vascularised organs in the body. Fluctuations in blood pressure, vascular spasms, and circulatory issues due to cholesterol or glucose imbalances all contribute to optic nerve atrophy. Thus, treating glaucoma involves more than just lowering eye pressure. It also includes managing hypertension, atherosclerosis, and neurological conditions. Your doctor will remind you of this during check-ups every three months.
Have there been any breakthrough technologies in the last decade that have been used to detect and stabilise the development of glaucoma?
Of course, new molecules and new drugs are emerging. The good thing is that many companies also operate in the Russian market. There are more high-quality domestic drugs, including cheaper ones for the patient. Today, we have a republican benefit for glaucoma patients — at the place of residence, a doctor prescribes a package of drugs that are free for a person for six months. This is, of course, wonderful. As for breakthroughs, new drugs are being released today, but we cannot say that they are much more effective than those that we used before. We have a fairly good set of medicines.
Laser technologies are becoming more and more popular and are increasingly being used in the treatment of glaucoma. We also have a technique for the initial stages of the disease (selective laser trabeculoplasty). These should be highly committed patients, because this treatment needs to be repeated at the right time. There is also a laser for advanced stages — laser cyclophotocoagulation, which we are increasingly using. The only thing is that the laser is slightly less effective than medical or surgical intervention.
New drains are appearing in surgery, which even allow for outpatient glaucoma surgery. Of course, their cost is quite high, but our pharmaceutical companies are already catching up and trying to produce more budget-friendly options that meet international standards.
“Meditation is part of the glaucoma treatment protocol in India”
Are there any ways to prevent glaucoma?
I think there is. Glaucoma is a disease that often develops against a background of stress. Stress can lead to mutations in cells, in cellular mitochondria. And this causes various diseases — for example, hypertension or the manifestation of diabetes mellitus. The same thing happens with glaucoma. All of these diseases have almost the same links of pathogenesis, but they appear in different places. The way to deal with the consequences depends on this: with diabetes, we reduce sugar, with hypertension, blood pressure and cholesterol, and with glaucoma, intraocular pressure.

Now people are more likely to live up to their illness. If, on average, one in four eighty-year-olds has glaucoma, then when we reach the age of 100, 50% of people with glaucoma will be among us.
Thus, it is necessary to minimise stress levels by all available means. By the way, meditation is part of the glaucoma treatment protocol in India. Stress tolerance and habituation to diseases should be formed in a child from childhood. There is no need to tell children that if they do well, they will never get sick. The ability to get sick should be formed from childhood. The ability to go to doctors, not to be afraid of them, to understand that a person is not perfect and that getting sick is a normal phenomenon for him. You just need to be able to be monitored and treated.
In addition, I will definitely mention a healthy lifestyle as a glaucoma prevention. The golden rules that everyone should use: quitting smoking, moderate cardio (walking, swimming, skiing, dancing). You do not need to lift a hundred—kilogram barbell, you should not dive or jump with a parachute — but feasible loads are absolutely necessary. Be sure to have a healthy, nutritious diet. It is imperative to sleep well — after 40 years of age, in general, one of the most important components of maintaining health. There must be positive socialisation in a person — communication with friends or in pleasant company develops cognitive functions of the brain. The older a person is, the more communication they need to have in order to keep their brain and psyche healthy.